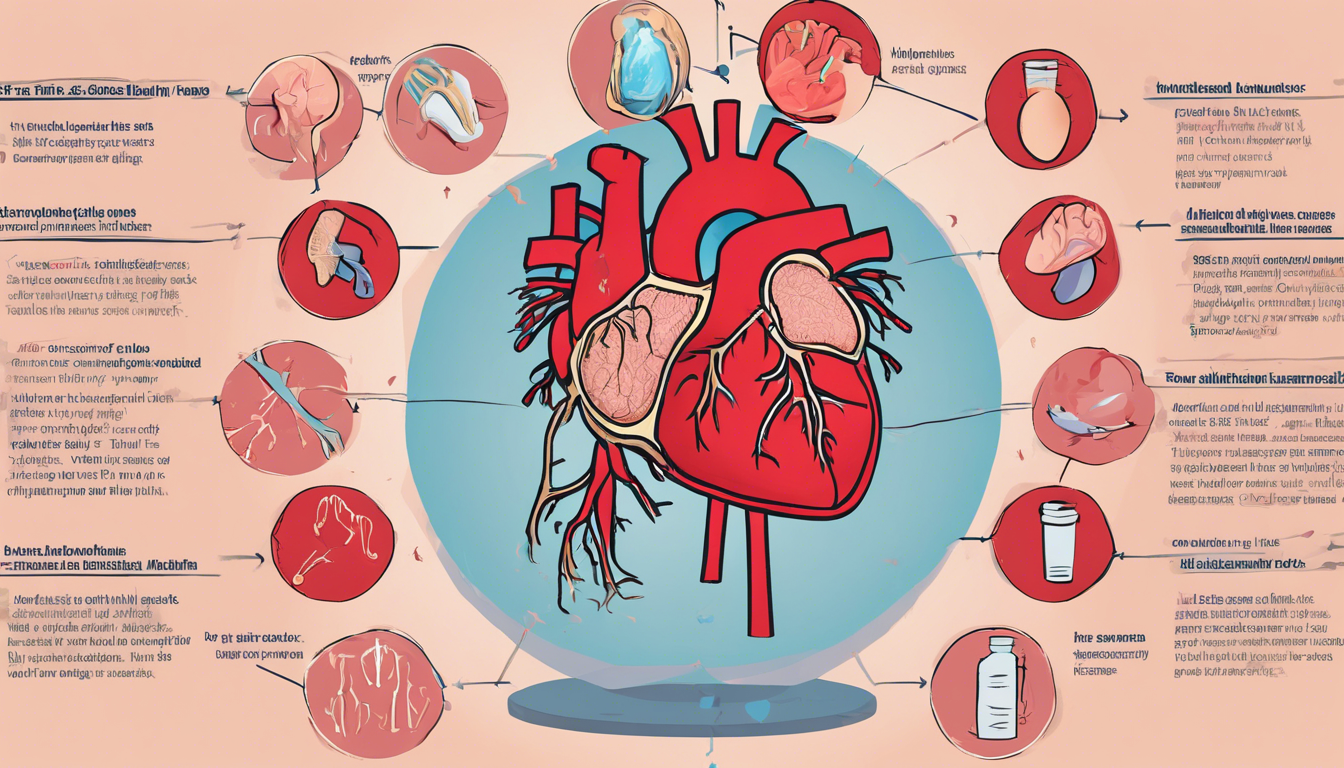
Understanding congestive heart failure (CHF), a significant and growing concern in the realm of cardiovascular diseases, is crucial for both patients and healthcare providers. This complex condition, often simply referred to using the chf medical abbreviation, goes beyond the heart’s inability to pump blood efficiently; it encompasses a wide spectrum of physiological challenges and impacts every aspect of a patient’s life.
With the increasing prevalence of heart failure symptoms and the detailed classification into stages, including the 4 stages of congestive heart failure and differentiation between left sided and right sided heart failure, the need for comprehensive information has never been more critical. Our exploration into what causes heart failure and how it’s defined underlines the importance of early recognition of symptoms such as swelling, fatigue, and shortness of breath – the hallmark signs of congestive heart failure.
In this article, we will delve into the heart of the matter, covering the full scope of congestive heart failure. We’ll start by unpacking the heart failure definition, aiming to illuminate the path from early signs of heart failure to the more advanced stages. A closer look at the causes reveals not only what causes CHF but also contributing factors that might exacerbate the condition. Diagnostic procedures play a pivotal role in managing heart failure, including the usage of the congestive heart failure icd 10 classification for precise documentation and treatment planning.
Treatment strategies for congestive heart failure aim to mitigate symptoms and improve quality of life, encompassing everything from lifestyle adjustments to medication and, in some cases, surgical interventions. By understanding both the symptoms of CHF and the comprehensive approaches to congestive heart failure treatment, our journey through this article promises to empower readers with knowledge and insight into managing this challenging condition effectively.
What is Congestive Heart Failure?
Congestive heart failure, often abbreviated as CHF, is a chronic condition where the heart’s ability to pump blood is inadequate to meet the body’s needs. Blood and fluids may accumulate in various parts of the body, leading to swelling and congestion, particularly in the lungs and legs. This condition can be life-limiting, requiring ongoing management through medications and other treatments to alleviate symptoms.
Explanation of the Condition
We understand congestive heart failure as a long-term issue where the heart struggles to pump efficiently. It does not signify that the heart has ceased functioning; rather, it cannot handle the volume of blood required, causing a buildup in other body parts, predominantly the lungs, legs, and feet. Various types of heart failure exist, including left-sided heart failure, right-sided heart, and high-output heart failure, the latter being quite rare.
Different Stages of Heart Failure
Heart failure progresses through several stages, from a high risk of developing the condition to advanced stages where symptoms significantly impact quality of life and may lead to frequent hospitalizations:
- Stage A: Individuals are at high risk but show no symptoms. Risk factors might include hypertension, diabetes, or family history of heart disease.
- Stage B: Known as pre-heart failure, where there is no symptom manifestation, but structural heart abnormalities or high filling pressures are present.
- Stage C: This stage involves individuals who have been diagnosed with heart failure and are experiencing symptoms or have a history of symptoms.
- Stage D: Represents advanced heart failure with severe symptoms that do not improve with standard treatments, often requiring more intensive management strategies.
Each stage requires specific considerations for treatment, aiming to manage symptoms and slow the progression of the disease effectively.
Common Causes and Contributing Factors
Heart-related Issues
We recognize that several heart-related conditions contribute significantly to the development of congestive heart failure. Predominantly, coronary artery disease (CAD) stands out as a primary factor. This condition arises from the buildup of fatty deposits in the arteries, which narrows them and reduces blood flow, potentially leading to a heart attack. Heart attacks themselves are acute events where an artery blockage leads to significant damage to the heart muscle, impairing its ability to pump effectively.
Additionally, heart valve disease and irregular heart rhythms (arrhythmias) also play critical roles. In cases where heart valves do not operate correctly, the heart must exert extra effort to pump blood, which can weaken it over time. Similarly, arrhythmias that cause the heart to beat too quickly or too slowly can strain the heart, leading to heart failure.
Non-heart-related Factors
Beyond direct heart-related issues, several other conditions and lifestyle factors contribute to the risk and exacerbation of heart failure. High blood pressure or hypertension is a notable contributor, making the heart work harder than normal, thereby increasing the risk of heart failure. Conditions such as diabetes, thyroid disorders, and kidney disease also place additional burdens on heart function.
Lifestyle choices and environmental factors are equally impactful. Smoking, physical inactivity, poor diet, and being overweight or obese are significant risk factors. These behaviors contribute to the development of heart-related issues that can lead to heart failure. Additionally, chronic diseases like HIV and the presence of autoimmune disorders or the buildup of substances like iron or protein can indirectly weaken heart function and contribute to heart failure.
In summary, the common causes of congestive heart failure stem from a combination of direct heart damage and the influence of external health and lifestyle factors. Managing these contributing factors is crucial for preventing the onset or worsening of heart failure.
Diagnostic Procedures
Initial Assessment
We begin the diagnostic process for congestive heart failure with a thorough initial assessment. This includes a detailed physical examination where our health care team listens to the heart and lungs using a stethoscope to detect any abnormal sounds, such as murmurs or irregularities. We also check for signs of fluid accumulation in the feet, ankles, and abdomen, which can indicate heart failure. Additionally, we assess the patient’s blood pressure and weight as these factors are crucial in diagnosing and managing heart failure.
A comprehensive review of the patient’s medical history, including any existing conditions like high blood pressure, coronary artery disease, or diabetes, is conducted. This review helps us understand potential risk factors that might contribute to heart failure. Moreover, blood tests are performed to measure levels of key substances such as electrolytes, creatinine, and specific proteins that indicate heart stress.
Advanced Diagnostic Tools
Following the initial assessment, we employ advanced diagnostic tools to further evaluate the heart’s condition and function. These include:
- Electrocardiogram (ECG): This test records the heart’s electrical activity and can help identify heart rhythm issues or the effects of a previous heart attack.
- Echocardiogram: Using sound waves, this test provides detailed images of the heart’s structure and function, helping us assess the heart’s pumping action and detect any abnormalities in the heart valves or chambers.
- Chest X-ray: X-rays help visualize the size and shape of the heart and lungs. This imaging is crucial in identifying signs of heart failure or other underlying conditions.
- Cardiac MRI and CT Scans: These imaging tests offer detailed views of the heart’s structure and function without using invasive procedures. They are instrumental in diagnosing complex heart conditions.
- Stress Tests: These tests measure the heart’s performance and blood flow while the patient is exercising to identify how well the heart handles activity.
- Cardiac Catheterization: A catheter is inserted into a heart artery to help pinpoint blockages that could be causing heart symptoms. This procedure also measures the pressures within the heart chambers.
- Biopsy and PET Scans: In certain cases, a small sample of heart tissue may be examined to diagnose specific heart muscle diseases. PET scans are utilized to observe the heart’s metabolic processes.
Each of these tools plays a pivotal role in our comprehensive approach to diagnosing congestive heart failure, allowing us to tailor treatment strategies effectively.
Managing Congestive Heart Failure
Treatment Protocols
We approach the treatment of congestive heart failure with a combination of pharmacological and non-pharmacological strategies. Medications play a crucial role and may include vasodilators to ease blood flow, diuretics for fluid retention, ACE inhibitors to improve heart function, and beta-blockers to enhance heart function and longevity. In severe cases, surgical interventions such as biventricular pacing therapy or heart transplantation may be necessary.
Lifestyle Modifications
Managing congestive heart failure also involves significant lifestyle adjustments. We advise our patients to adopt heart-healthy habits to alleviate symptoms and slow disease progression. Key recommendations include:
- Dietary Adjustments: Reducing sodium intake is essential to prevent fluid buildup. We often suggest following a Mediterranean or DASH diet, which are linked to reduced heart failure incidents and may protect against disease progression.
- Physical Activity: Regular, moderate-intensity exercise is encouraged to strengthen the heart. Specific programs may be recommended based on individual health status.
- Weight Management: Maintaining a healthy weight is crucial as excess weight can strain the heart.
- Fluid Intake Monitoring: Monitoring and possibly restricting fluid intake can be important, especially in severe cases or those with hyponatremia.
- Smoking and Alcohol: Quitting smoking and limiting alcohol consumption are advised to reduce heart strain.
- Stress Management: Techniques for managing stress and anxiety, which can exacerbate heart failure symptoms, are recommended.
- Sleep Quality: Addressing sleep disorders such as sleep apnea is important as they can impact heart failure.
By integrating these treatment protocols and lifestyle modifications, we aim to manage congestive heart failure effectively, improving both the quality of life and survival rates for our patients.
Conclusion
Through this comprehensive exploration of congestive heart failure, we’ve traversed the intricacies of its causes, symptoms, and the multifaceted approach required for effective management. From understanding the initial signs and the critical importance of early diagnosis to delving into the detailed treatment options and the essential lifestyle changes necessary for mitigation, we’ve underscored the significant impact that informed, proactive participation can have on managing this condition. The emphasis on advanced diagnostic tools and the personalized treatment strategies highlights the evolution of care tailored to improve patient outcomes and quality of life.
Recognizing the complexity of congestive heart failure not only demands a nuanced approach to treatment but also a commitment to ongoing research and adaptation of care practices. As we’ve discussed, the integration of medication, lifestyle adjustments, and possible surgical interventions plays a pivotal role in managing the symptoms and progression of this condition. This article serves as a testament to the power of knowledge and the critical importance of collaborative care strategies in confronting congestive heart failure, encouraging patients and healthcare providers alike to engage in a continuous dialogue about the most effective practices for care and management.
FAQs about Congestive Heart Failure (CHF)
1. What are the stages of congestive heart failure (CHF) and how are they classified?
Congestive heart failure progresses through stages A to D:
- Stage A: High risk without symptoms.
- Stage B: Structural heart abnormalities without symptoms.
- Stage C: Symptoms present or history of symptoms despite treatment.
- Stage D: Advanced symptoms requiring specialized, often intensive care. Classification helps tailor treatment to manage symptoms and slow progression effectively.
2. What are the common causes of congestive heart failure (CHF)?
Several factors contribute to CHF:
- Heart-related issues: Coronary artery disease, heart attacks, and heart valve diseases.
- Non-heart-related factors: Hypertension, diabetes, obesity, and lifestyle choices like smoking and physical inactivity. Identifying and managing these factors is crucial in preventing and managing CHF.
3. How is congestive heart failure (CHF) diagnosed and what diagnostic tools are used?
Diagnosis involves a comprehensive assessment:
- Physical examination to detect abnormal heart sounds and fluid accumulation.
- Medical history review to assess risk factors.
- Advanced tools such as echocardiograms, ECGs, and cardiac MRI to evaluate heart structure and function.
- These tests help confirm CHF, determine its severity, and guide treatment decisions effectively.




1 Comment